“Minimally invasive spine surgery has emerged as a truly game-changing option for patient’s requiring spine surgery. The selective removal and/or reconstruction of the responsible spinal pathology while preserving normal tissues minimizes risk, maximizes benefits and affords a far more comfortable surgical experience and recovery. -Less can be more…a lot more – Now that is smart surgery!”
Spine Problems are Common, and Some Will Require Surgical Treatment
Virtually everyone will have one or more episodes of back or neck pain at some point in their lives. In fact, the problem of back pain is so common that fully one quarter of the U.S. population will report an episode of back pain in the last three months, and an additional 15% of the population will report an episode of neck pain during the same time frame. For the majority, this will be a short lived event that will predictably resolve on its own. For many others, however, one or more treatments, including chiropractic care, physical therapy, weight loss, massage, acupuncture, medications (anti-inflammatories, muscle relaxants) and spinal steroid injections (“pain shots”) will prove helpful in expediting recovery. For the remaining few who fail these measures and in whom pain and other symptoms persist, surgery be the most appropriate, and in some instances, the only meaningful option.
All too often, patients are understandably fearful of spine surgery, as the mere mention of the word conjures distressing images of big incisions, prolonged hospitalizations, immobility, and slow painful recoveries. With the development of minimally invasive spine surgery options, however, many patients will now enjoy a far more comfortable surgical experience, with smaller incisions, shorter hospital stays, far less pain, and a much faster return to normal life than was ever thought possible with traditional methods. So if you have been suffering from back and neck pain where nothing seems to be working, and you have been contemplating a neurosurgical solution, then read on, because minimally invasive spine surgery may be right for you.
Less is More
The past few years have seen major technical and conceptual advancements in the field of spinal neurosurgery. An emerging philosophical change is that less is often more. Traditional spine surgery involved large incisions, disruption of delicate muscles, and damage to ligaments and other stabilizing soft tissues, all of which were stripped aside in order to expose and correct a diseased spine. The trauma of the surgery, once considered unavoidable, constituted a form of “friendly fire” that undermined the quality of the surgical result, led to prolonged periods of convalescence, postoperative pain and a slower return to normal activities.
To circumvent this problem, our approach to spine surgery has been minimized, both in concept and in technique. The surgical objective is to identify and correct the cause of symptoms while painstakingly preserving remaining structures, both anatomically and functionally. Although this requires significantly greater preoperative planning, a thorough knowledge of microsurgical anatomy and spine biomechanics, and is far more technically demanding than traditional surgical approaches, the results for the patient are well worth the additional effort. It is important to reiterate that the goals of minimally invasive surgery is to accomplish the same clinical objectives as the traditional open approach, but without the extensive tissue trauma.
There are three essential elements to planning and execution of minimally invasive spine surgery.
Precise identification of the surgical target (the problem):
In order to correct any spinal disorder, the precise site of the problem needs to be rigorously determined. Very often, MRIs will show several sites of disease and/or multiple levels of degeneration, but amid these, it is usually one particular level and/or a single anatomic structure (bulging disc, bony spur, facet joint, nerve root, etc.) that is responsible for most or all of the symptoms. By carefully listening to the patient’s symptoms, performing a detailed neurological exam, and meticulously correlating these findings with the patient’s imaging studies, the precise surgical target that is generating the patient’s symptoms can usually be identified, no matter how “noisy” the MRI scan might seem. This is a critical step because each patient is unique and the surgical solution needs to individualized to each patient’s unique pathology. In this way, minimally invasive surgery is “smarter” and more selective than the more generic traditional surgical approaches.
Planning the least invasive corridor of surgical access (the path):
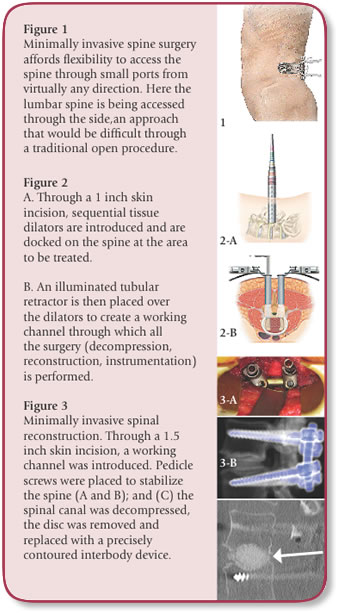
Once the surgical target has been mapped, I plan the smallest, safest, and most direct physiologic corridor of access, which can be from the front, the side, the back, or along any 360 degree trajectory about the spine (figure 1). Aside from a small skin incision, no other normal structures are cut. Small tissue dilators are introduced and easily pass between muscles by gently dilating the muscle fibers rather than dividing them. Tubular retractors or ports are docked on the spine and serve as the working channel through which all the surgery is microscopically performed (figure 2).
Reconstruction of the spine (the final product):
Many spinal procedures not only involve taking pressure off of the nerves (decompression), but also involve restoring stability of a diseased spine (reconstruction). Reconstruction is performed through the same illuminated working channels, and involves the placement of implants. These can be composed of bone, plastic, acrylic, or metal and are used to replace, fuse, or otherwise stabilize a diseased disc segment, or an entire vertebral body. The addition of metal screws, small rods or plates can further restore stability to the spine (figure 3). In many instances, we use a computerized navigational guidance system to precisely deploy these implants into the spine with millimeter accuracy.
What Conditions can it be Used for?
Minimally invasive spine surgery is my preferred choice for most forms of spine surgery including most degenerative conditions (disc herniations, disc degeneration, spinal stenosis, bony spurs, spondylolisthesis, spinal instability, and nerve root compression), as well as in many situations requiring complex reconstruction and fusion. I will also use it selectively in cases of scoliosis, spinal tumors, and in some forms of spine trauma/fractures. In general, the indications for minimally invasive surgery are similar to those where traditional “open” surgery is currently being used.
What are the Benefits?
The benefits are many, including smaller incisions, less blood loss, reduced infection rate, shorter hospital stays, faster recovery and much less pain. Most of my patients, including those in whom complex reconstructions and fusions are performed, will be up and walking within hours of the procedure and are typically home after a brief 1-2 day hospital stay.
Minimally Invasive Spine Surgery and the Aging Spine
Minimally invasive spine surgery is effective for adults of all ages, but its merits are especially well received among the elderly. First, degenerative spinal conditions such as spinal stenosis are most common in the elderly population. Furthermore, many elderly patients have multiple underlying medical problems including osteoporosis and heart disease that can prove prohibitive to the large open spine surgeries. With minimally invasive spine surgery, blood loss and normal tissue disruption is minimized, reducing the physiologic burden of surgery and enhancing its safety. Furthermore, the rapid mobilization and reduced reliance on postoperative pain medications are additional virtues of the procedure among the elderly.
For most os us, periodic episodes of back and neck pain will be a self-limited phenomena for which a variety of nonsurgical options will prove effective, if, however, back and neck problems persist to the point where neurologic function is threatened, mobility is impaired, pain is intractable and/or quality of life is compromised, a neurosurgical solution may warrant serious consideration.